Article sections
- Abstract
- Etiology
- Screening
- Treatment
- References
Amblyopia (lazy eye) is decrease in best corrected visual acuity in one or both eyes and is not due to any structural abnormality of the eye. It develops during childhood and results in interruption of normal cortical visual pathway development, as a result visual acuity reduces. In amblyopia there is abnormal visual processing of primary visual cortex.1 Prevalence of amblyopia is 1-5 % worldwide.2-4 The World Health Organization (WHO) estimates 19 million children less than 15 years of age are visually impaired, of those 12 million are impaired due to amblyopia and uncorrected refractive error.
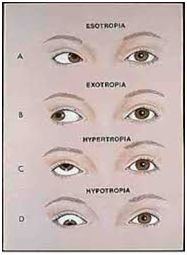
Amblyopia may occur as early as first week of life. If visual pathway to the visual cortex are not properly stimulated, visual cortex cannot mature properly. 5A number of ophthalmic conditions can cause amblyopiai.e strabismus (ocular misalignment), refractive errors (anisometropia). Strabismus is the most common contributing factor. Amblyopia develops in deviating eye, which may turn inward, outward, upward, downward. Small intermittent deviations are rarely associated with amblyopia.
Refractive error is the second most contributing factor to the development of amblyopia. It is divided into two types: anisometropia and isometropia. Anisometropic amblyopia develops when refractive error in two eyes are unequal. It causes the image to be out of focus on the retina, effecting visual pathway in that eye. Severe refractive error in both eyes, may cause bilateral isometropic amblyopia. The least common amblyogenic condition, congenital or acquired media opacities cause deprivation amblyopia. Cataract, corneal lesions or ptosis block retinal image formation and cause amblyopia.
Early screening in amblyopia results in better outcomes.6 Regular school visits of eye practitioners and examination of visual acuity of children can screen out amblyopia.
The diagnosis of amblyopia is made when there is reduction in visual acuity that is not due to any physical abnormalities, structural eye pathology (optic nerve or macular lesions) or abnormalities of visual pathway. Snellen chart, HOTV, tumbling E chart are used for examination. If visual acuity of 20/20 is not achieved on routine vision screening, then pinhole testing may be used to determine whether vision corrects or not. If visual acuity improves it indicate refractive error. If not amblyopia must be considered.7 The corneal light reflex text may be performed at any age and can be used to detect strabismus. Reflex goes opposite to the site of deviation.
Treatment of amblyopia depends on its cause. It was thought that treatment was a little benefit after age 10 years but recent studies showed that visual acuity can improve in adolescence8. Refraction is done to the best corrected visual acuity and the child is prescribed glasses. In children with strabismus, the most common technique is to stimulate amblyopic eye by placing a patch over the good eye for a specific period each day. Additional treatment include wearing opaque contact lens over good eye. Another alternative is penalization therapy with installing atropine drops in good eye. This blurs vision and amblyopic eye is used. Both patching and penalization are effective.

Uncategorized References
1. Levi DM. Linking assumptions in amblyopia. Vis Neurosci. 2013;30(5-6):277.
2. Aldebasi YH. Prevalence of amblyopia in primary school children in Qassim province, Kingdom of Saudi Arabia. Middle East African journal of ophthalmology. 2015;22(1):86.
3. Fu J, Li SM, Liu LR, Li JL, Li SY, Zhu BD, et al. Prevalence of amblyopia and strabismus in a population of 7th-grade junior high school students in Central China: the Anyang Childhood Eye Study (ACES). Ophthalmic Epidemiol. 2014;21(3):197-203.
4. Ganekal S, Jhanji V, Liang Y, Dorairaj S. Prevalence and etiology of amblyopia in Southern India: results from screening of school children aged 5–15 years. Ophthalmic Epidemiol. 2013;20(4):228-31.
5. Epelbaum M, Milleret C, Buisseret P, Duffer JL. The sensitive period for strabismic amblyopia in humans. Ophthalmology. 1993;100(3):323-7.
6. Williams C, Northstone K, Harrad RA, Sparrow JM, Harvey I. Amblyopia treatment outcomes after screening before or at age 3 years: follow up from randomised trial. BMJ. 2002;324(7353):1549.
7. Practice CO, Medicine A. Eye Examination in Infants, Children, and Young Adults by Pediatricians. Pediatrics. 2003;111(4 Pt 1):902-7.
8. Scheiman MM, Hertle RW, Beck RW, Edwards AR, Birch E, Cotter SA, et al. Randomized trial of treatment of amblyopia in children aged 7 to 17 years. Archives of ophthalmology (Chicago, Ill: 1960). 2005;123(4):437-47.
9. Group PEDI. A randomized trial of atropine regimens for treatment of moderate amblyopia in children. Ophthalmology. 2004;111(11):2076-85. e4.
10. Group PEDI. The course of moderate amblyopia treated with patching in children: experience of the amblyopia treatment study. Am J Ophthalmol. 2003;136(4):620-9.
Mahnoor asif
Bsc(hons) optometry King Edward medical university, COAVS
Member of Pascal medical mission organization