What is schizophrenia:
Schizophrenia is a serious mental disorder in which people interpret reality abnormally. Schizophrenia may result in some combination of hallucinations, delusions, and extremely disordered thinking and behavior that impairs daily functioning, and can be disabling.
Theoretical Researches on Schizophrenia:
A study from Harvard Medical School, the Broad Institute and Boston Children’s Hospital has shown that the risk of schizophrenia increases if a person inherits specific variants in a gene related to “synaptic pruning” the elimination of connections between neuron. The findings were based on genetic analysis of nearly 65,000 people. The study represents the first time that the origin of this psychiatric disease has been causally linked to specific gene variants and a biological process. It also helps explain two decades-old observations: synaptic pruning is particularly active during adolescence, which is the typical period of onset for symptoms of schizophrenia, and the brains of schizophrenic patients tend to show fewer connections between neurons. The gene, complement component 4 (C4), plays a well-known role in the immune system. It has now been shown to also play a key role in brain development and schizophrenia risk. The insight may allow future therapeutic strategies to be directed at the disorder’s roots, rather than just its symptoms. Research has shown that Schizophrenia afflicts approximately 1 percent people worldwide and is characterized by hallucinations, emotional withdrawal and a decline in cognitive function. These symptoms most frequently begin in patients when they are teenagers or young adults.
Sally Shepherd, Colin A. Depp, Gloria Harris, Maureen Halpain, Lawrence A. Palinkas, Dilip V. Jeste has done qualitative research on Perspectives on schizophrenia over a lifespan which was published in March, 2012. In this article the traditional view of schizophrenia has been that of progressive decline yet cross sectional or longitudinal studies indicate substantial heterogeneity in the long-term course of schizophrenia. The aim of this study was to gain an understanding of the perspectives of older adults with schizophrenia about if and how their experience of the illness had changed over the lifespan as well as their expectations for the future. Study participants were recruited from the database of the University of California, San Diego (UCSD) Advanced Center for Innovation in Services and Intervention Research that focuses on late-life psychoses, and is funded by the National Institute of Mental Health. Participants were recruited by informing other Center investigators of the study and through dissemination of study information via Center recruitment staff a total of 32 individuals were scheduled and interviewed. The minimum age to participate in the study was 50 years. After providing informed consent, participants were interviewed at UCSD or at their place of residence, depending on their preference. The meeting consisted of a semi structured interview and a demographic questionnaire. The interview was developed in collaboration with 2 community members (a consumer [S.S.] and the parent of a consumer [G.H.]) and 2 academic researchers (C.D., M.H.). The community members held leadership roles in the San Diego Affiliate of the National Alliance on Mental Illness. All interviewers, including community members, attended two 3-h training meetings which covered the goals of the project procedures, interviewing techniques, participant and interviewer safety. The interviews were designed to be open-ended so that interviewees could elaborate on other areas that they felt were important to describing schizophrenia over their lifespan. Data analysis to be done by the three interviews were randomly selected and coded independently by the coders to estimate interceder reliability. Initially, the percent agreement between coders was 60%, but upon inspection, a large proportion of the disagreements were found to lie in the assignment of time frame, specifically pre diagnosis and diagnosis until the present. Once these 2 codes were merged, the percent agreement was 75%, indicating an acceptable degree of concordance between coders 27 of them. the mean age of the sample was 55.7 years (SD = 4.1 years; range 50–72). Median income fell below the poverty line (<$10 000), and only 13.3% of participants were currently employed. Participants had experienced the symptoms of schizophrenia for, on average, 35 years. Codes were identified representing life domains as well as the 3 lifespan segments (onset and early course, middle course, current, and future outlook). Using these codes and the constant comparison technique, themes emerged within the sections of the semi structured interview. We assessed these themes with respect to perceived changes over time in the course of illness.
Causes of schizophrenia:
- The exact causes of schizophrenia are unknown.
- Data from modern scientific research proves that schizophrenia is unequivocally a biological disease of the brain, just like Alzheimer’s Disease and Bipolar Disorder.
- For one thing, schizophrenia is now known to be partially caused by genetics and to be inherited.
Schizophrenia as biological diseases:
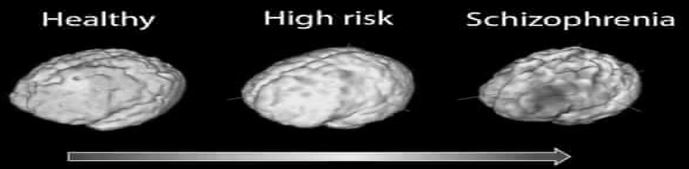
- Magnetic Resonance Imaging (MRI) and Computerized Tomography (CT), have documented structural differences between schizophrenic and normal brains.
- Individuals with schizophrenia have up to 25% less volume of gray matter in their brains, especially in the temporal and frontal lobes (known to be important for coordination of thinking and judgment).
- Patients demonstrating the worst brain tissue losses also tend to show the worst symptoms.
- Functional scanning of the brain, using technologies like Positron Emission Tomography (PET) and functional MRI have made it possible to create real-time maps of regional cerebral blood flow and metabolism, providing another window into how schizophrenic brains are distinct from normal brains.
- Such studies tend to show low levels of activation in schizophrenic patients’ middle frontal cortex and inferior parietal cortex compared to normal people included as control subjects.
- Low activity findings like this are also correlated with (related to) increased negative symptoms (meaning that people who tend to have more negative symptoms, also tend to show lower levels of brain activity in key brain areas).
Connection between schizophrenia and neurotransmitters:
There’s a connection between neurotransmitters and schizophrenia because drugs that alter the levels of neurotransmitters in the brain are known to relieve some of the symptoms of schizophrenia. Schizophrenia may be caused by a change in the level of 2 neurotransmitters that are dopamine and serotonin.
Functional disturbance:
Functional disturbances of the brain have also been connected with frontal and temporal structures in some schizophrenic patients. Of the single neurotransmitter substances, dopamine and serotonin appear to represent some of the central restitutive mechanisms whose function is to maintain mental stability; the understanding of their interplay with other neurotransmitters such as noradrenaline, acetylcholine, GABA, and glutamate, should provide a more integrated view of both normal and disturbed brain function. Neuro-anatomical and neuro-morphological data have revealed ventricular enlargement and diminished frontal and temporal lobe volume in some patients. These changes are concentrated particularly in the hippocampus/ parahippocampal gyrus/amygdala, but are relatively small and span some overlap with healthy subjects.
Twin studies suggest that at least some of these changes may result from other than genetic factors. relatively small and span some overlap with healthy subjects. Twin studies suggest that at least some of these changes may result from other than genetic factors.
Abnormalities in sensory processing:
Abnormalities in sensory processing are also evident in schizophrenic patients. It is common for schizophrenic patients to show ‘soft’ neurological signs, meaning that they might have difficulty distinguishing between two simultaneous touches or in being able to identify numbers drawn on the palm of their hand. They also tend to confuse the right and left sides of their bodies more frequently than normal people. Such well documented observations of sensory processing problems suggest impairments or irregularities in the way that schizophrenics’ brains are wired. Still more evidence of neurological impairment in schizophrenia comes from consideration of electroencephalogram (EEG) data, which are tests of brain electrical activity. About one-third of schizophrenic people show abnormal electrical brain impulses, also suggesting irregularities in the way schizophrenic brains are wired. Considered as a whole, these numerous and methodologically distinct results suggest converging and compelling evidence for the idea that schizophrenia is basically a biologically based brain disease.
Diagnosis for Schizophrenia:
- Physical examination
- Tests and screenings
- Psychiatrists’ evolution
- Diagnosis criteria for schizophrenics (DSM-5)
Treatments for the Schizophrenia:
Medications and therapies are used for the purpose of managing symptoms of Schizophrenia. Different types of psychotherapies which are used for managing symptoms.
- Cognitive Behavioral Therapy (CBT)
- Individual Therapy
- Cognitive Enhancement Therapy (CET)
Different Types of Psychosocial Therapies also used during psychotherapy sessions which included: –
- Social Skill Training
- Rehabilitation
- Family education
- Self-help Group
- Coordinate specialty Care (CPC)
- Assertive Community Treatment (ACT)
- Social Recovery Therapy (SRT)
Medication for schizophrenia patients:
Different medication used for treatment is Second Generation antipsychotic Drugs, First Generation antipsychotic Drugs and Electroconvulsive Therapy (ECT).
References
Biedermann, F. & Fleischhacker, W. (2016). Psychotic disorders in DSM-5 and ICD-11. CNS Spectrums. 21 (4): 349–54.
Eisenberg DP. & Berman KF. (2010). “Executive function, neural circuitry, and genetic mechanisms in schizophrenia”. Neuropsychopharmacology. 35 (1): 258–77.
Nakata Y. Kanahara N. & Iyo M. (2017). “Dopamine super sensitivity psychosis in schizophrenia: Concepts and implications in clinical practice”. Journal of Psychopharmacology (Oxford, England). 31 (12): 1511–1518.
Tandon R., Gaebel W. &Barch DM, (2013). Definition and description of schizophrenia in the DSM-5. Schizophrenia Research. 150 (1): 3–10.